Achieving Health Care Justice: Breaking Down Racial Disparities in Health Care
Written by:
University of Tulsa
• Dec 20, 2023

Achieving Health Care Justice: Breaking Down Racial Disparities in Health Care
Black mothers in the U.S. are more likely to die from pregnancy-related causes than mothers in other racial or ethnic groups. Native Hawaiian and other Pacific Islander mothers are up to four times more likely to get late or no prenatal care compared to mothers in other racial and ethnic groups. In 2021, the overall life expectancy in the U.S. was 76.1 years, but the life expectancy for American Indians and Alaska Natives was 65.2 years.These striking figures reflect systemic issues woven into the fabric of the U.S. health care system. Beyond data points, these numbers tell the story of real people grappling with the life and death consequences of racial disparities.
By championing health care justice, health care professionals can begin to dismantle the structures that perpetuate disparities. They can then build a system where everyone gets the care they deserve.
Understanding Health Care Inequities
The aspiration of health care justice is that every person gets a fair and equitable opportunity to reach their optimal level of health. An individual’s race, socioeconomic status, educational attainment, gender, or sexuality should not determine whether they have access to cancer screenings or insulin to control their diabetes. Nor should such factors influence the quality of care they receive.
Health care justice means that all individuals, regardless of their background, have equal access to:
- Preventive care
- Affordable medications and treatments
- Inclusive health education
- Timely emergency care
- Fair representation in clinical trials
- Culturally competent mental health services
- Quality maternal care that addresses disparities in maternal mortality rates
- Opportunities to lead healthy lifestyles
Unfortunately, this vision of health care justice has yet to be fulfilled. A host of inequities persists, and some groups unnecessarily experience higher rates of poor health and early death.
These avoidable differences often run along racial lines and arise from social, economic, or systemic factors that create unfair advantages or disadvantages for different groups. A comprehensive understanding of these disparities in health and health care, however, can serve as a vital step toward dismantling the barriers obstructing health equity .
Consider the following aspects of health care where disparities can appear:
- Health outcomes: Differences in the incidence, prevalence, and severity of diseases or health conditions among different racial or ethnic groups
- Health care access: Variances in the ability of individuals from different racial backgrounds to access medical care, preventive services, and essential treatments
- Quality of care: Discrepancies in the standard of health care provided to individuals based on their race, leading to variations in treatment plans, medications, and medical procedures
- Health care utilization: Differences in patterns of health care utilization, including disparities in the frequency of medical visits, screenings, and preventive care
Socioeconomic Status and Health
Socioeconomic factors play a key role in people’s ability to access quality health care. Data has consistently shown links between socioeconomic status and health in communities and revealed that individuals with lower incomes often face:
- Higher rates of uninsurance
- Limited access to preventive care
- Lack of a regular source of care
These conditions can result in delayed diagnoses, preventable complications, and poor health.
For example, studies have shown that a low socioeconomic status puts people at greater risk of developing and dying of heart disease . Research has also shown that a person’s socioeconomic status strongly predicts their likelihood of getting diabetes .
The Intersection of Socioeconomics and Race
Centuries of systemic racism that have denied financial opportunities to racial and ethnic minorities still influence today’s economic landscape. Inequalities in income, education, and employment status persist along racial and ethnic lines, as do other factors that determine a person’s socioeconomic status.
Data from the U.S. Census Bureau and U.S. Bureau of Labor Statistics highlight some of these inequalities:
- Black individuals make up 13.5% of the total U.S. population but represent 20% of those living in poverty.
- Hispanic individuals of any race make up 19.3% of the total U.S. population but represent 28.4% of those living in poverty.
- The share of American Indians and Alaska Natives living in poverty is about two times higher than their share of the total population.
- The median salary of Black workers is approximately 19% less than that of white workers.
- The median salary of Latino workers is about 22% less than that of white workers.
These socioeconomic gaps faced by racial and ethnic minorities affect more than their economic well-being. They also negatively impact their health by influencing their ability to engage in healthy activities, afford medical care, and manage stress, which all can contribute to poor health outcomes.
Unequal Access and Health Care Inequities
While health care justice focuses on achieving equal access to quality care for everyone, a long history of health care inequities has led to significant gaps in people’s health, drawn along racial lines. Inequities that have perpetuated these gaps include the following.
Referral Inconsistencies
Referrals to specialists provide patients with critical access to specialized medical care. Timely referrals can make all the difference when it comes to ensuring patients receive prompt diagnoses and appropriate treatments.
When patients do not receive appropriate referrals it can result in delayed diagnoses, preventable complications, and an unequal quality of care.
A recent study examined the referral patterns of primary care providers , specifically to pulmonary, cardiology, gastroenterology, orthopedics, general surgery, and neurology specialists. The findings show significant statistical differences in the number of referrals made for white and Black patients, suggesting a stark contrast in Black patients’ access to specialized care.
Diagnostic Disparities
Unequal access to timely and accurate diagnoses disproportionately affects certain racial groups. For example, the study “ Racial Disparities in Diagnostic Delay Among Women With Breast Cancer ” found the following disparities:
- Black women were twice as likely to face delays in getting a diagnostic evaluation, delays in getting a biopsy, and total delays of 45 days or more, compared to white women.
- Women who experienced delays of 45 days or more had a 1.6 times higher chance of dying from breast cancer compared to those without delays in their diagnosis.
Varied Treatment Options
Patients from racial and ethnic minorities may find themselves offered suboptimal treatment options for the same condition compared to other patients. Factors unrelated to the actual medical needs of the patient often account for these discrepancies in care.
As an example, disparities in access to health information, particularly for minority populations, may mean that patients are not fully informed about all their available treatment options. This lack of information can limit their ability to advocate for themselves in the health care decision-making process.
Whatever the specific reason, examples of patients from racial and ethnic minorities being offered fewer treatment options abound. A recent Centers for Disease Control and Prevention (CDC) report, for instance, found the following racial disparities in the treatment of mild-to-moderate cases of COVID-19 that had a high risk of becoming severe:
- The antiviral medication Paxlovid, used to prevent the progression of COVID-19, was prescribed to Black patients 35.8% less often than it was prescribed to white patients.
- American Indian or Alaska Native and Native Hawaiian or other Pacific Islander patients and Asian patients also faced lower Paxlovid prescription rates, 23.1%, and 19.4% less often, respectively.
- Hispanic patients were prescribed Paxlovid 29.9% less often than non-Hispanic patients.
Surgical Disparities
Patients from racial and ethnic minorities are less likely to receive potentially lifesaving and life-improving surgical interventions than their white counterparts. Health care providers often steer these patients toward less invasive procedures.
Research published in JAMA Surgery reveals a consistent pattern : White patients undergo major surgeries to treat everything from coronary artery disease to appendicitis to knee joint damage at higher rates compared to Black patients.
For example, white male patients were 131% more likely to receive knee replacement surgery than were Black male patients.
The Consequences of Racial Disparities in Health Care
Racial disparities in health care have translated into poor health outcomes for people belonging to racial and ethnic minority groups, from lower life expectancies to higher rates of chronic health problems. These disparities represent the tangible impact of systemic inequities on the health and well-being of individuals within these communities, and addressing them is critical to achieving health care justice
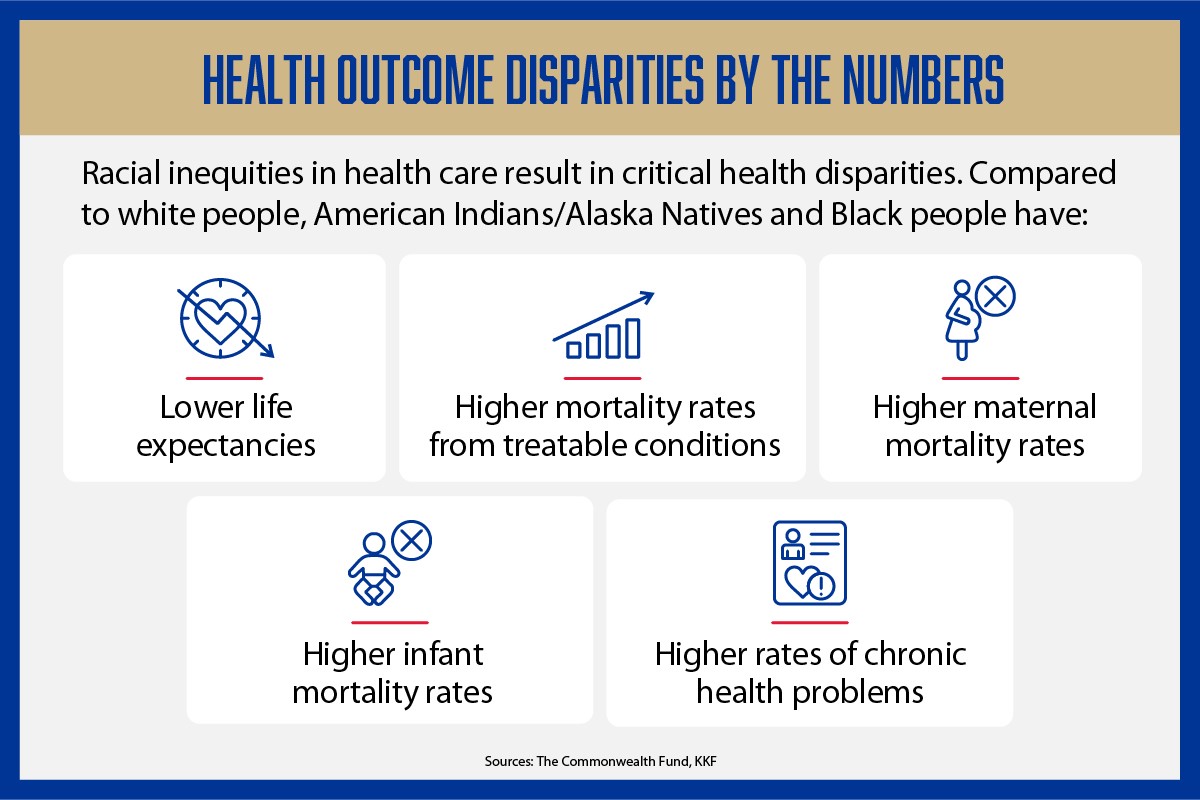
Racial inequities in health care result in critical health disparities. According to The Commonwealth Fund and KKF, compared to white people, American Indians/Alaska Natives and Black people have: lower life expectancies, higher mortality rates from treatable conditions, higher maternal mortality rates, higher infant mortality rates, and higher rates of chronic health problems.
Life Expectancy Disparities
Life expectancy can serve as a critical metric for understanding the overall health and well-being of different racial groups.
CDC data from 2021 reveals stark contrasts in life expectancy among racial groups:
- American Indians/Alaska Natives: 65.2 years
- Black people: 70.8 years
- White people: 76.4 years
Life expectancies were particularly low for Black males (66.7 years) and American Indian/Alaska Native males (61.5 years).
Between 2019 and 2021, Americans’ overall life expectancy declined by 2.7 years. However, the following notable variations in life expectancy declines further highlight the disparities among racial and ethnic groups:
- American Indians/Alaska Natives experienced the largest decline, 6.6 years.
- Hispanic and Black people faced declines of 4.2 and 4.0 years, respectively.
- White people experienced a smaller decline, 2.4 years.
- Asian people had the smallest decline, 2.1 years.
Racial Disparities in Mortality Rates From Treatable Conditions
When left untreated, certain health conditions can lead to serious problems and even death. But timely access to top-notch health care can allow people to effectively manage or even prevent these health conditions altogether.
People with diabetes, for example, can effectively manage their condition with consistent monitoring and medications. However, the following mortality rates for various treatable conditions by race underscore the significant disparities.
Diabetes
Mortality rates for diabetes in 2021 were twice as high for American Indians/Alaska Natives, Native Hawaiians/other Pacific Islanders, and Black people compared to white people . Hispanic people were 1.3 times more likely to die from diabetes than white people.
Breast Cancer
Breast cancer is considered treatable when detected early. However, Black people, often diagnosed at later stages of their disease, exhibit much higher rates of breast cancer mortality compared to people in other racial or ethnic groups.
Maternal Mortality Disparities
The loss of mothers during or shortly after childbirth can reveal much about a community’s health and the effectiveness of its health care system. This health indicator speaks not only to the quality of medical care during pregnancy and delivery but also to the broader social factors influencing mothers’ well-being.
The numbers elucidate stark disparities.
Data from 2021 shows Black women were 2.6 times more likely to die from pregnancy-related issues and childbirth compared to white women. Additionally, from before the COVID-19 pandemic to after it, maternal mortality rates for Hispanic women rose by nearly 20% between 2019 and 2021 .
Compared to white women, Black, American Indian/Alaska Native, and Native Hawaiian/other Pacific Islander women exhibit higher rates of:
- Preterm births: Preterm infants are at increased risk for developmental challenges, respiratory issues, and infections.
- Low birth weight births: Low birth weight infants have a higher risk of infections and are more susceptible to developmental problems. Low birth weight is also associated with an increased risk of death.
- Births with late or no prenatal care: A lack of consistent care and monitoring can result in missed opportunities for early detection and intervention for mothers and babies with potential health issues.
While only 4% of white women give birth having had late or no prenatal care, this is the reality for other women:
- American Indian/Alaska Native mothers: 12%
- Black mothers: 9%
- Hispanic mothers: 8%
Racial Disparities in Infant Mortality Rates
Despite overall improvements in infant mortality rates, glaring disparities persist, revealing a concerning trend in the health outcomes of newborns from different racial backgrounds. The 2020 infant mortality rate , a record low overall, masks a troubling reality — infants born to women of color face significantly higher risks of mortality compared to those born to white women.
In 2020, the infant mortality rate for Black infants stood at 10.4 per 1,000 live births, more than two times higher than that of white infants, who had a rate of 4.4 per 1,000. American Indian/Alaska Native and Native Hawaiian/other Pacific Islander infants experienced mortality rates nearly twice as high as white infants, with rates of 7.7 and 7.2 per 1,000, respectively.
The Asian community showed the lowest infant mortality rate at 3.1 per 1,000 live births, signaling a potential area for insights into factors contributing to better outcomes. However, these variations highlight the urgent need to address the root causes of the disparities that persist.
Racial Disparities in Rates of Chronic Health Problems
Several factors can increase a person’s risk of developing a chronic disease such as asthma, cancer, cardiovascular disease, or diabetes. In addition to a person’s genetics and age, common risk factors include an unhealthy diet and lifestyle, chronic stress, and environmental factors such as exposure to pollutants and toxins.
Addressing these risk factors through patient education, health initiatives that support healthy lifestyles, and regular medical check-ups can help reduce the burden of chronic diseases on individuals and communities.
Persistent racial disparities in the rate of chronic health problems highlight the need for aggressive efforts toward achieving health care justice. Consider the prevalence of various chronic diseases among different racial and ethnic groups , as of 2021.
Diabetes rates:
- Black adults: 16%
- Hispanic adults: 12%
- American Indian/Alaska Native adults: 15%
- White adults: 11%
Asthma rates:
- Black adults: 12%
- American Indian/Alaska Native adults: 13%
- Hispanic adults: 8%
- Native Hawaiian/other Pacific Islander adults: 6%
- Asian adults: 6%
- White adults: 10%
Asthma rates in children:
- Black children: 17%
- White children: 9%
The disparities extend beyond specific diseases. Consider the racial breakdown of adults concurrently experiencing three or more chronic health conditions , such as arthritis, cancer (not including skin cancer), asthma, chronic obstructive pulmonary disease, chronic kidney disease, cardiovascular disease, depression, and diabetes:
- Black adults: 10.7%
- Multiracial adults: 14.1%
- American Indian/Alaska Native adults: 18.4%
The Role of Nurses in Advancing Health Care Justice
The nursing profession has a rich history of advocating for health care justice and striving toward greater equity. From the early pioneers to modern-day practitioners, nurses have played a pivotal role in challenging systemic injustices and promoting inclusivity.
With the inception of modern nursing, Florence Nightingale pushed for improvements in patient care and emphasized the importance of providing holistic care that addressed both the physical aspects of illness and the psychological needs of patients. This set a precedent for the role of patient advocacy in nursing.
Throughout the years since, nurses have used their voices to challenge discriminatory practices and champion the rights of marginalized communities. During the Civil Rights Movement, Mabel Keaton Staupers , a leader in the National Association of Colored Graduate Nurses, worked tirelessly to end racial discrimination in nursing education and employment. This paved the way for a more diverse and inclusive nursing workforce.
In more recent decades, nurses have played key roles in the struggle to address the health care needs of the LGBTQIA+ community. The American Nurses Association (ANA) has developed reports and guidelines, such as the Nursing: Scope and Standards of Practice guidebook , that advocate for culturally competent and LGBTQIA+-inclusive care.
Recognizing the importance of cultural competence in health care, nurses have pushed for education and training that goes beyond clinical skills. Efforts to integrate cultural competence into nursing curricula and professional development programs reflect a commitment to providing care that respects patients’ diverse backgrounds.
Nurses are poised to play a pivotal role in advancing health care justice over the next decade. In particular, nurse leaders stand to make a significant impact on improving equitable access to quality health care for all individuals.
Unleashing this potential requires concerted efforts to address the barriers constraining nurses from working to the full extent of their education and training. This includes revising scope-of-practice laws, shaping public health policies, and influencing health system policies.
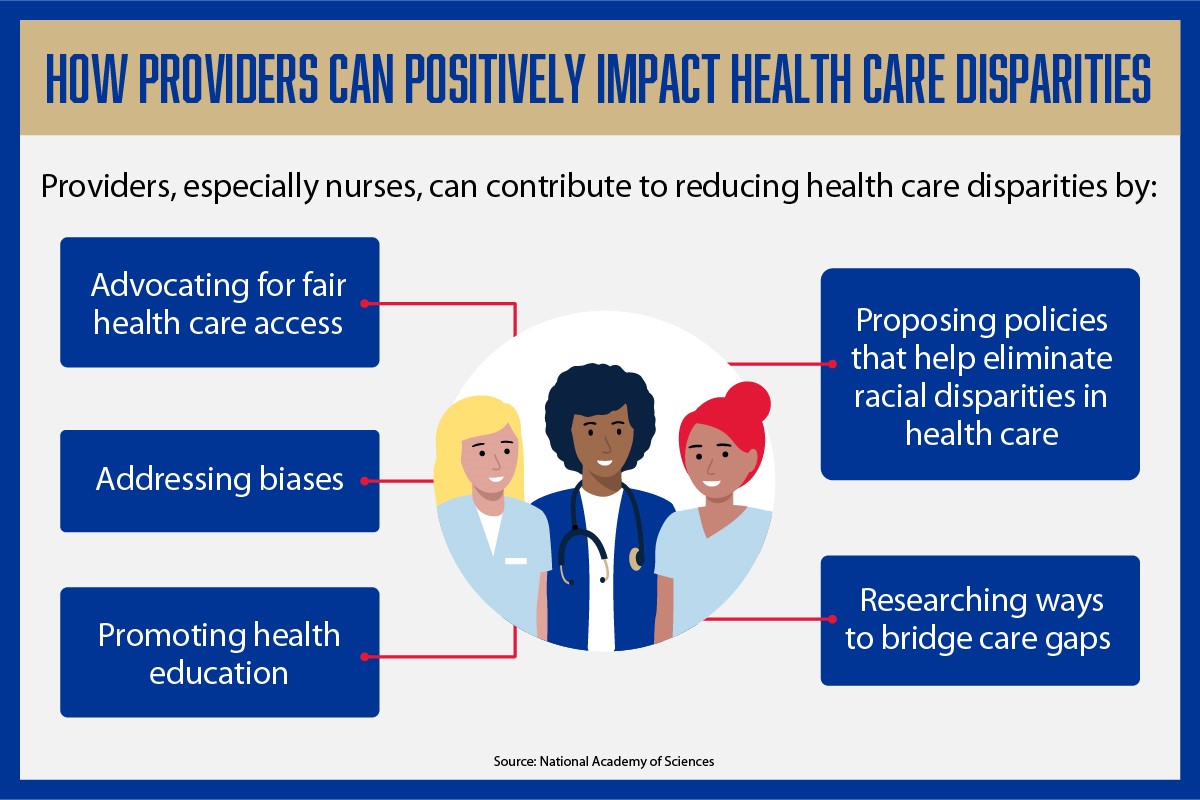
According to the National Academy of Sciences, providers, especially nurses, can contribute to reducing health care disparities by: advocating for fair health care access, addressing biases, promoting health education, proposing policies that help eliminate racial disparities in health care, and researching ways to bridge care gaps.
Advocating for Fair Health Care Access
A productive discussion about effective ways to advocate for equitable health care access first requires recognition of the disparities embedded in health care access . Gaining access to the health care system requires insurance, provider availability, and proximity to a health care provider. However, other factors such as economic instability, discrimination, and educational disparities can also get in the way of people accessing needed health care.
While health care may address patients’ immediate needs, it falls short of mitigating the root causes of health disparities. Nurses have a unique role in addressing both patient symptoms and the societal issues affecting their patients’ health. These include the following:
-
Revising scope-of-practice laws: Restrictive scope-of-practice laws limit nurses’ autonomy to fully utilize their nursing skills. This places constraints on nurses’ capacity to provide holistic patient care and best address broader social factors that significantly impact their patients’ health.
When scope-of-practice laws are changed to be more aligned with nurses’ training and expertise, nurses can fill gaps in care and increase patients’ ability to access health care , especially in areas with a shortage of health care providers. Additionally, less restrictive scope-of-practice laws allow nurses to contribute significantly to primary care, chronic disease management, and preventive services.
-
Community partnerships: Through their roles and responsibilities, nurses can connect and align the health care services they provide with the needs and dynamics of the communities they serve. For example, after identifying a rising diabetes trend in their community, nurses can initiate a program that addresses patients’ clinical needs and connects individuals with vital social support.
Nurses play a crucial role in ensuring that health care practices are not isolated from the social, cultural, and economic contexts of the communities in which they operate. This involves acknowledging and addressing the unique challenges, disparities, and social factors impacting patients’ health within their communities.
Addressing Biases
Biases impact health outcomes. They can manifest in various ways — from delayed diagnoses to differences in treatment recommendations. For example, racial biases are likely responsible for the well-documented undertreatment of pain in Black patients .
Addressing biases requires introspection and education. Nurses can seek cultural competency training to learn about the diverse backgrounds of the patients they serve. By actively working to eliminate their biases, nurses contribute to a health care system that treats every patient with the same level of care and attention, regardless of their racial or ethnic background.
However, biases are deeply ingrained in the health care system and often go beyond individual attitudes. To tackle the larger problem, nurses can advocate for institutional policies that promote equity, diversity, and inclusion. This involves pushing for fair hiring practices, culturally sensitive care protocols, and ongoing education for health care professionals to continuously challenge and overcome their biases.
Promoting Health Education
Health education can be a powerful tool for reducing racial health disparities and advancing health care justice. Low health literacy can limit people’s ability to obtain health-related information, correctly use medications, and follow guidance from health care professionals. Promoting health education helps increase access to vital health information about everything from family planning to signs of depression.
Nurses, often at the front line of patient care, have a unique opportunity to bridge educational gaps about health and health care. By serving as educators in health care settings, they can engage patients from diverse racial backgrounds in meaningful conversations about their health.
Additionally, nurses can tailor health education initiatives so they resonate with people from varied backgrounds. This can involve creating educational materials that are linguistically accessible, culturally sensitive, and attuned to the specific health challenges faced by different racial groups.
Such initiatives can extend beyond hospital walls and into communities where nurses can conduct health education workshops that empower individuals with the knowledge they need to make informed decisions about their health.
Proposing Policies That Tackle Racial Disparities in Health Care
As front-line health care providers, nurses witness the impact of systemic inequities on patients’ health. This positions nurses to advocate for policy changes and draw attention to the prevalent racial disparities in health care.
To propose effective policies, nurses need to target the root causes of specific racial disparities they hope to bring attention to. This will likely involve advocating for policies that address both the socioeconomic factors and the systemic racism that impact people’s health.
In these efforts, collaboration is key. Nurses need to work with policymakers, researchers, and community leaders, sharing their insights and experiences along the way as policies take shape. Additionally, nurses can advance their proposals by collaborating with researchers and using health care data to pinpoint areas needing improvement. This evidence can serve as the catalyst for policy discussions and, ultimately, positive change.
Bridging Care Gaps Through Research
Research can play a key role in bridging care gaps. This in turn can help further the cause of health care justice and shape evidence-based practice in nursing that can help mitigate disparities and improve health outcomes. Additionally, research empowers health care professionals and policymakers to make informed decisions, ensuring that strategies to bridge care gaps are grounded in data rather than assumptions.
Priorities nurses may consider in their research projects include:
- Identifying where care gaps exist
- Directly involving patients in the research process to ensure efforts are tailored to their community’s needs
- Exploring innovative technologies that can potentially narrow gaps in care delivery
- Assessing the quality of care provided across different racial and ethnic groups
- Focusing on socioeconomic factors, geographical challenges, and cultural influences that contribute to care gaps
- Concentrating on translating research on care gaps into practical applications
Dismantle Racial Disparities in Health Care for a More Just Future
In the quest for health care justice, dismantling racial disparities is a shared responsibility. It calls for reform, for a health care landscape where everyone receives equitable care, regardless of their race or ethnicity.
As advocates for change, health care professionals — and, particularly, nurses — have the power to reshape the country’s health care system to one that truly prioritizes the well-being of every individual and champions a healthier and more just future for all.