The Team Nursing Model: What It Is and How It Improves Care
Written by:
University of Tulsa
• Mar 6, 2024

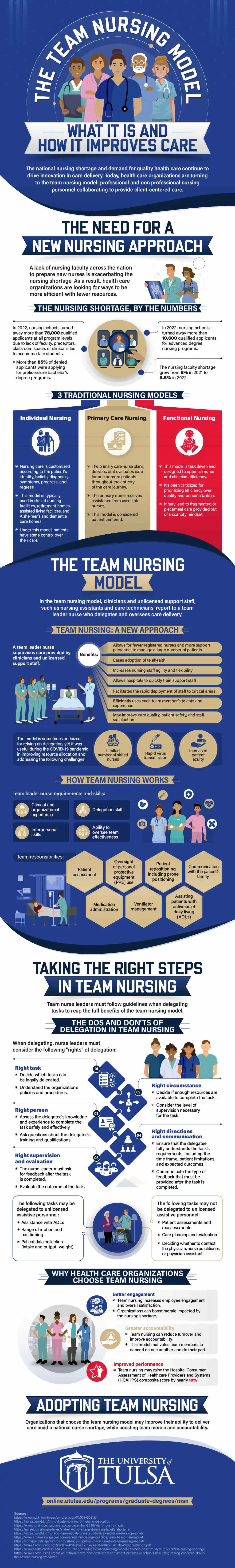
The national nursing shortage and demand for quality health care continue to drive innovation in care delivery. Today, health care organizations are turning to the team nursing model: professional and nonprofessional nursing personnel collaborating to provide client-centered care.
To learn more, check out the infographic created by the online Master of Science in Nursing (MSN) program at The University of Tulsa.
The Need for a New Nursing Approach
A lack of nursing faculty across the nation to prepare new nurses is exacerbating the nursing shortage. As a result, health care organizations are looking for ways to be more efficient with fewer resources.
The Nursing Shortage, by the Numbers
In 2022, nursing schools turned away more than 78,000 qualified applicants at all program levels due to lack of faculty, preceptors, classroom space, or clinical sites to accommodate students. More than 85% of denied applicants were applying for prelicensure bachelor’s degree programs. In addition, nursing schools turned away more than 10,600 qualified applicants for advanced degree nursing programs. The nursing faculty shortage grew from 8% in 2021 to 8.8% in 2022.
Traditional Nursing Models
Individual nursing is a model in which nursing care is customized according to the patient’s identity, beliefs, diagnosis, symptoms, progress, and regress. This model is typically used in skilled nursing facilities, retirement homes, assisted living facilities, and Alzheimer’s and dementia care homes. Under this model, patients have some control over their care.
In the patient-centered primary care nursing model, the primary care nurse plans, delivers, and evaluates care for one or more patients throughout the entirety of their care journeys. The primary nurse receives assistance from associate nurses.
The functional nursing model is task driven and designed to optimize nurse and clinician efficiency.
However, the model has been criticized for prioritizing efficiency over quality and personalization. This approach may lead to fragmented or piecemeal care provided out of a scarcity mindset.
The Team Nursing Model
In the team nursing model, clinicians and unlicensed support staff, such as nursing assistants and care technicians, report to a team leader nurse who delegates and oversees care delivery.
Team Nursing: A New Approach
A team leader nurse supervises care provided by clinicians and unlicensed support staff. Team nursing allows for fewer registered nurses and more support personnel to manage a large number of patients. It eases the adoption of telehealth and increases nursing staff agility and flexibility. Team nursing allows hospitals to quickly train support staff and facilitates the rapid deployment of staff to critical areas. The model efficiently uses each team member’s talents and experience and may improve care quality, patient safety, and staff satisfaction.
Team nursing is sometimes criticized for relying on delegation, yet it was useful during the COVID-19 pandemic in improving resource allocation and addressing numerous challenges, including a limited number of skilled nurses, rapid virus transmission, and increased patient acuity.
How Team Nursing Works
For team nursing to work, the team leader must have clinical and organizational experience, delegation skills, interpersonal skills, and the ability to oversee team effectiveness.
Team responsibilities include patient assessment; medication administration; oversight of personal protective equipment (PPE) use; ventilator management; patient repositioning, including prone positioning; assisting patients with activities of daily living (ADLs); and communication with the patient’s family.
Taking the Right Steps in Team Nursing
Team nurse leaders must follow guidelines when delegating tasks to reap the full benefits of the team nursing model.
The Dos and Don’ts of Delegation in Team Nursing
When delegating, nurse leaders must consider the following “rights” of delegation. They must decide which tasks can be legally delegated and understand the organization’s policies and procedures.
The right circumstance requires deciding if enough resources are available to complete the task and considering the level of supervision necessary for the task.
The right person must determine if the delegatee has the knowledge and experience to complete the task safely and effectively. The right person must also ask questions about the delegatee’s training and qualifications.
The right directions and communication include ensuring that the delegatee fully understands the task’s requirements, including the time frame, patient limitations, and expected outcomes. In addition, nurse leaders must communicate the type of feedback that must be provided after the task is completed.
Finally, the right supervision and evaluation require the nurse leader to ask for feedback after the task is completed and evaluate the outcome of the task.
The tasks that may be delegated to unlicensed assistive personnel include assistance with ADLs; range of motion and positioning; and patient data collection, such as intake and output (I&O) and weight.
The tasks that may not be delegated to unlicensed assistive personnel include patient assessments and reassessments; care planning and evaluation; and deciding whether to contact the physician, nurse practitioner, or physician assistant.
Why Health Care Organizations Choose Team Nursing
Team nursing increases employee engagement and overall satisfaction. This model may enable organizations to boost morale impacted by the nursing shortage.
Team nursing can reduce turnover and improve accountability by motivating team members to depend on one another and do their part.
Team nursing may raise the Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) composite score by nearly 10%, a sign of improved performance.
Adopting Team Nursing
Organizations that choose the team nursing model may improve their ability to deliver care amid a national nurse shortage, while boosting team morale and accountability.
Please add No-Follow HTML markup for hyperlinks in the sources section.
Sources
American Association of Colleges of Nursing, Nursing Faculty Shortage Fact Sheet
American Medical Association, Team-Based Care Model
Community Hospital Corporation, “Stronger Together: The Value of a Team Nursing Model”
HealthLeaders, “How A Team-Based Nursing Model Can Help Offset Today’s Nursing Shortage”
Nursa, “Nursing Care Models: Primary, Individual, and Team Nursing”
Nursa, “What Is Nursing Delegation, and What Are the 5 Rights of Delegation?”
NursingCenter, “Team Nursing Model – What It Is and How to Make It Work”


